Cardiovascular diseases: the essential circulation in danger
Cardiovascular diseases are among the most dangerous consequences of aging. In 2014, they even caused 46% of deaths in Europe[1]! But what are cardiovascular diseases?
These are all diseases that affect our cardiovascular system, i.e. our heart, arteries or veins. As explained in part 1 on anemia, our circulatory system is essential to the delivery of oxygen in our bodies. But how does it work? It is organized into two loops, one pulmonary and one systemic, connected by an organ: the heart. The heart acts as a pump, which sends blood to the lungs (lung loop), where it fills with oxygen and empties of accumulated carbon dioxide. The heart then recovers the blood and directs it to the rest of the body (systemic loop).
Inside these loops, blood leaves the heart through the arteries. It carries out exchanges (gas, nutrients) with the body via the capillaries. Finally, it returns to the heart through the veins. The cardiovascular system therefore has a crucial role in body-wide communication. Unfortunately, aging does not spare it. In this article we will first look at what atheroma is, one of the main causes of age-related cardiovascular disease. We will then discuss the various diseases and damage that it can cause, before discussing the simple actions that can reduce the risk of suffering from them.
Cardiovascular diseases and aging: atheroma, a recurrent culprit in age-related cardiovascular disease
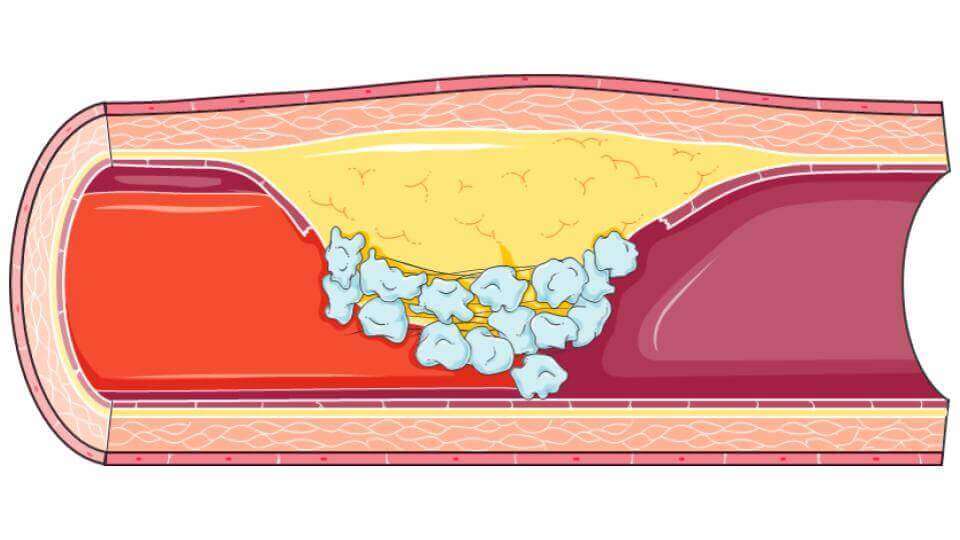
Atheroma is defined as a plaque essentially composed of fat on the walls of the arteries[2]. As we will see, these plaques can play many roles, whether by clogging arteries or dangerously weakening their walls. Its formation is slow, and is done in several stages that we will detail here.
Cardiovascular diseases and aging: a breach in the system
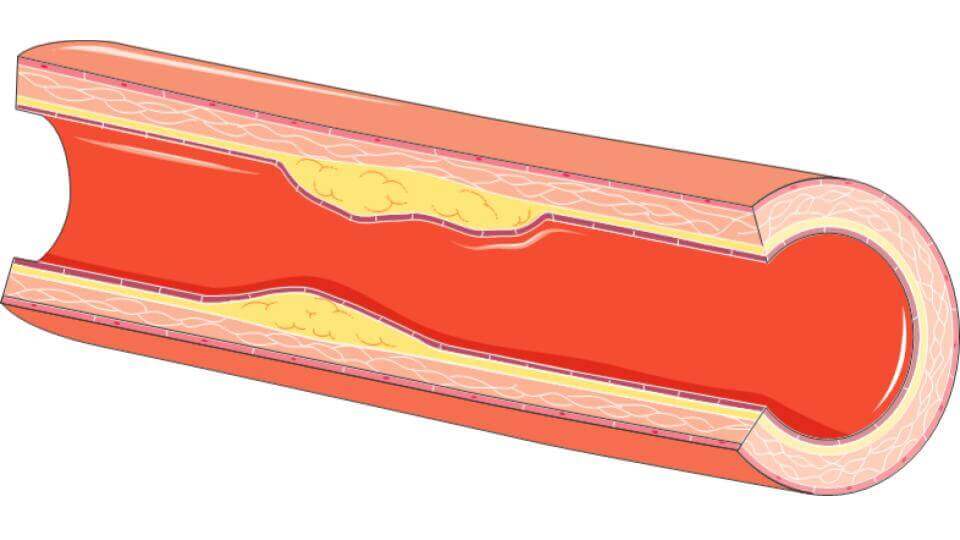
Among the nutrients transported by the blood are fats. These are condensed with proteins to form so-called lipoproteins (LPs). They will be the main cause of atheromas. However, for the plaque of fat to form, something must hold it in place. Indeed, the image of fat deposits being made directly on the surface of the artery, often used, is not really accurate. To settle, fats need to pass under the first layer of cells from inside the artery, the endothelium[3]. In some areas of the arteries, it is weakened and does not perform its role as a barrier to perfection. It is in these areas that LPs will be able to infiltrate[4]. It is then assumed that these first infiltrations would start a chain reaction, further weakening the endothelium[5]. This is the first step in the formation of the fat plaque: atheroma.
Cardiovascular diseases and aging: infiltration, then inflammation
In our bodies, when something is not right, the immune system is most often used. This is exactly what the cells of the infiltrated endothelium do. They then attract a particular type of immune cell: monocytes[6]. Once at the infiltration site, the environment pushes the monocytes to transform into “cleaning” cells: macrophages[7]. These cells then begin to digest the LPs to convert them back into cholesterol, so that they can be evacuated and the fat plaque destroyed[8].
The inflammation also recruits cells from inside the aorta, the fibroblasts, which then try to heal the lesion[9]. This prevents the platelets in our blood from coming into contact with the injured area, which could cause clots to form. Thus, most of the atheromas that form in our arteries are either destroyed or contained. They therefore do not lead to any complications afterwards. However, sometimes not everything goes as planned.
Cardiovascular diseases and aging: faulty inflammation
Aging is often defined as the accumulation of lesions that our bodies cannot repair. Atheroma is a good example. Indeed, sometimes the inflammation that is supposed to cleanse the atheroma degenerates. Macrophages, by consuming LPs, become intoxicated. The consequences are then dramatic. Intoxicated macrophages accumulate, in addition to LPs, inside the atheroma. By dying, without being destroyed by other macrophages in the same state as them, they form what is called a necrotic body[8].
The atheroma then continues to grow, but also to weaken. Indeed, intoxicated macrophages produce molecules capable of digesting the fibrous matrix protecting the atheroma, which can lead to a leakage of its contents into the bloodstream[10].
These are the two consequences of atheroma, which are so dangerous for health. First, the swelling, which clogs the artery, is called stenosis. The second is the direct consequence of the release of its content into the blood. This content is immediately recognized as a foreign body by the platelets in our blood, which triggers a coagulation process. Huge clots form and that’s what we call thrombosis.
Cardiovascular diseases and aging: a wide range of serious consequences
Depending on the part of the cardiovascular system affected by atheromas, the consequences differ. We will distinguish among these, those affecting the arteries of the heart, the brain and finally those of the rest of the body.
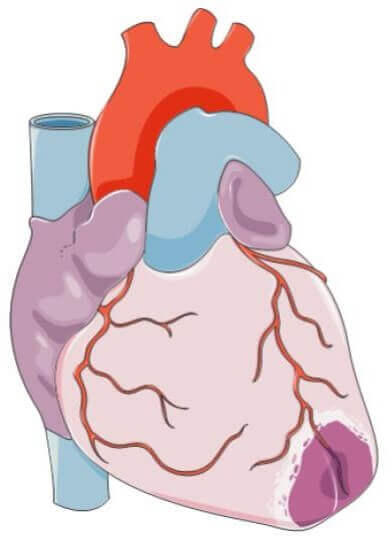
Cardiovascular diseases and aging: coronary heart disease, when the heart no longer irrigates itself

The heart is certainly not a muscle like any other, but it still needs significant amounts of oxygen to ensure its role as a pump of the blood system. For this purpose, it is richly supplied by many blood vessels. These include coronary arteries and, like all arteries, coronaries can develop atheromas. The health consequences are then serious.
If the atheroma gradually clogs the coronary arteries (stenosis process), it causes what is called angina. The heart is insufficiently supplied with blood and malfunctions[11]. The patient experiences severe pain of varying duration in the chest, but may radiate to the left arm, shoulders or even the jaw[12].
These symptoms should not be taken lightly. Indeed, as we have seen previously, atheroma causes artery stenosis but can develop into thrombosis. If the atheroma in the coronary artery ruptures, a clot can form and suddenly block the artery. Part of the heart then no longer receives any blood at all: the atheroma has caused a myocardial infarction, or heart attack[13]. The consequences are much greater than for angina pectoris. The area affected by the heart attack is not only dysfunctional, it can become necrotic if the clot remains in place for too long. Instead of dead muscle cells, scar tissue will form, which does not provide at all the contractile functions of the heart[14]. The pain felt during heart attacks is severe, affecting the same areas as the pain caused by angina, but lasting more than 20 minutes[15]. In 10% of cases, myocardial infarction is still fatal today[16].
Cardiovascular diseases and aging: cerebrovascular diseases, when the brain suffocates
To function properly, our brain consumes large amounts of energy and oxygen. Thus, it is richly vascularized to allow this supply. A supply whose cessation can have serious consequences. Unfortunately, with age, the probability of incidents increases[17]. It has been shown that in more than 50% of fatal cases of stroke, cerebral atheromas were present[18].
There are two processes leading to these disorders: either the vessels are blocked or they are broken inside the brain. In the first case, this blockage may occur in a similar way to what has just been described for coronary heart disease. Blockage is most often the result of stenosis or thrombosis[19], with atheroma as a possible cause[20].

In the second case, when a vessel ruptures, it is called cerebral hemorrhage. This is most frequently caused by what is called an aneurysm[21]. An aneurysm is a deformation of a weakened artery, which will form a sort of pocket, which, if left untreated, eventually ruptures and causes internal bleeding[22]. Atheromas are one of the major causes of artery fragility leading to aneurysms.
The consequences of these strokes are variable. They depend on the location and size of the area that has been affected, with different cognitive and motor aspects that can be affected. In addition, the length of time the area has been without supply also counts. If it is short enough, the neurons may have survived for the most part. The consequences of stroke range from virtually no damage, to death. At the end of the 1990s, 70% of stroke patients did not survive more than 5 years[23].
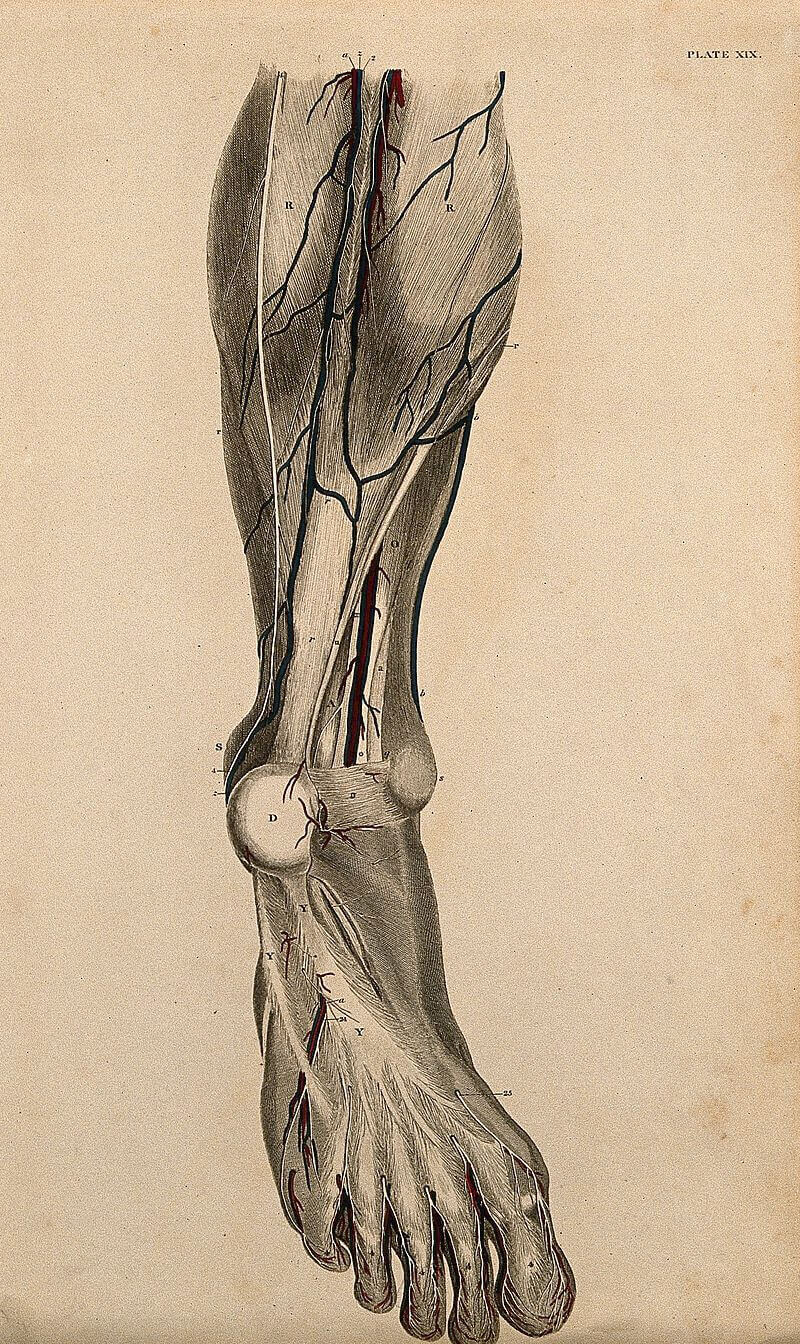
Cardiovascular diseases and aging: the rest of the body is not spared
It is not only the heart and brain that are vulnerable to cardiovascular disease. The lower limbs are also often affected. An example of cardiovascular disease affecting them is obliterating arteriopathy of the lower limbs. This is a direct consequence of the formation of an atheroma in the vessels that irrigate the legs[24]. The limbs no longer receive blood, and the consequences for the patient can be very uncomfortable: at best, limping, at worst, skin ulceration which can even lead to necrosis of the limb with the need for amputation[25].
The other condition that affects the lower limbs often has nothing to do with atheroma. It is called phlebitis, or deep vein thrombosis. As its name suggests, it is the formation of clots in the veins. The reason for the formation of these clots is not yet fully explained[26]. The direct consequences are often unpleasant but benign: pain, swelling, swelling, swelling of the leg veins…[27] However, if the clot migrates, the consequences can be much more serious.
The elastic structure of the veins can allow the clot to move to the heart, where it can send the clot into the pulmonary arteries. This can then create a pulmonary embolism[28]. In this case, the patient instantly feels short of air, coughs, sometimes even coughs blood[29]. This is due to the sudden loss of irrigation to part of the lungs, where blood will then accumulate. If the clot remains in place, a lung infarction is even possible, with part of it even necrotizing[30]. It is also reported that 15% of sudden deaths observed are due to pulmonary embolism[31].
Cardiovascular diseases and aging: simple actions to reduce risks
We have just seen the different consequences of cardiovascular disease, but how can we avoid becoming a victim? Most cardiovascular diseases related to aging are related to the formation of atheromas. It appears that the best way to prevent this is to reduce the probability of formation and magnification of these plaques[32]. Their main formation factors are hypertension, which weakens the artery and allows LPs to seep into the artery[33], as well as too high blood sugar levels and of course the presence of large quantities of LPs in the blood[34]. Fortunately, there are many ways to reduce these factors. Here are a few examples.
Adapt your lifestyle

Regular exercise has been shown to be an excellent way to reduce the risk of cardiovascular disease[35]. This is more than understandable: sport can reduce the risk of high blood pressure by working the heart constantly and regulating blood pressure, and the consumption of LPs by increasing their use during exercise. For the same reasons, it has been shown that avoiding being overweight is also an obvious good solution[36].
Another way to reduce both hypertension and the amount of circulating LPs is to adopt certain dietary habits. Thus, reducing the amount of sugars and saturated fatty acids and increasing the consumption of fruits, vegetables and seeds is a good method to reduce the risk of cardiovascular disease[37].
One of the most well-known and easily avoidable risk factors is tobacco consumption[38]. The reason is simple: tobacco consumption, through the action of nicotine on our brains, causes a vascular signal that increases blood pressure[39] and thus weakens the arteries.
To avoid cardiovascular diseases, it is also not recommended to consume large quantities of alcohol. Indeed, alcohol has pro-coagulant properties that would increase the damage in the event of thrombosis. Nevertheless, although controversial, results would show that low alcohol consumption would have a protective effect against these diseases[40].

Preventive treatments exist for cardiovascular diseases

Even before developing a cardiovascular disease, if a patient is predisposed for it, he or she can undergo preventive treatments. Treatments exist to reduce the amount of fat circulating in the blood. Statins are molecules that are already used for this purpose to prevent the risk of cardiovascular disease[41].
The other widely used method is to prescribe drugs to patients to lower their blood pressure. Many analyses agree on the effectiveness of this method, regardless of the molecule used for treatment[40].
In conclusion, cardiovascular diseases are diseases whose incidence increases sharply as we get older. As we have seen, these are many and they can affect most of our organs. However, their causes are often similar and the atheroma we have described extensively is one of the most common causes. It is thus thanks to the joint progress of scientific research and medicine that today it is possible to reduce to a minimum the risks of suffering the consequences. If we applied all the simple principles to avoid them, would it be possible for their omnipresence to disappear from the future of our society?
Diseases of aging: our articles
Baptiste Tesson

Author
Auteur
Baptiste is studying biology at the École Normale Supérieure de Lyon and bioengineering at the École Polytechnique Fédérale de Lausanne. He worked on the optimization of Cas9 as a tool for genome editing and on the emergence of blood stem cells in the zebrafish. He currently works on the patterning of the muscles, also in the zebrafish. He plans on doing a PhD in developmental biology.
More about the Long Long Life team
Baptiste étudie la biologie à l’École Normale Supérieure de Lyon et la bioingénierie à l’École Polytechnique Fédérale de Lausanne. Il a travaillé sur l’optimisation de la protéine Cas9 comme outil de modification de génomes et sur le développement des cellules souches du sang chez le poisson zèbre et travaille actuellement sur la mise en place des muscles chez le même animal. Il projette de réaliser un doctorat axé vers le développement animal.
En savoir plus sur l’équipe de Long Long Life
References
[1] Nichols M, Townsend N, Scarborough P, Rayner M, Cardiovascular disease in Europe 2014: epidemiological update, Eur Heart J, 2014;35:2950-2959
[2] https://www.inserm.fr/information-en-sante/dossiers-information/atherosclerose
[3] Williams KJ, Tabas I. The Response-to-Retention Hypothesis of Early Atherogenesis. Arteriosclerosis, thrombosis, and vascular biology. 1995;15(5):551-561.
[4] Tabas I, García-Cardeña G, Owens GK. Recent insights into the cellular biology of atherosclerosis. The Journal of Cell Biology. 2015;209(1):13-22. doi:10.1083/jcb.201412052.
[5] Tabas I1, Williams KJ, Borén J.Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation. 2007 Oct 16;116(16):1832-44
[6] Mestas, J., and Ley, K. (2008). Monocyte-endothelial cell interactions in the development of atherosclerosis. Trends Cardiovasc. Med. 18, 228–232.
[7] Johnson, J.L., and Newby, A.C. (2009). Macrophage heterogeneity in atherosclerotic plaques. Curr. Opin. Lipidol. 20, 370–378.
[8] Moore KJ, Tabas I. The Cellular Biology of Macrophages in Atherosclerosis. Cell. 2011;145(3):341-355. doi:10.1016/j.cell.2011.04.005.
[9] Libby P (2002). “Inflammation in atherosclerosis”. Nature. 420 (6917): 868–74.
[10] Galis, Z.S., Sukhova, G.K., Lark, M.W., and Libby, P. (1994). Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J. Clin. Invest. 94, 2493–2503.
[11] Dimitris Tousoulis, Emmanuel Androulakis, Anna Kontogeorgou, Nikolaos Papageorgiou, Marietta Charakida, Katerina Siama, George Latsios, Gerasimos Siasos, Anna-Maria Kampoli, Panagiotis Tourikis, Kostas Tsioufis and Christodoulos Stefanadis. Current Pharmaceutical Design (2013) 19: 1593.
[12] Talbert RL. Chapter 23. Ischemic heart disease. In: Talbert RL, DiPiro JT, Matzke GR, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York, NY: McGraw-Hill; 2011
[13] Reed, Grant W; Rossi, Jeffrey E; Cannon, Christopher P (January 2017). “Acute myocardial infarction”. The Lancet. 389 (10065): 197–210.
[14] Britton, the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston ; illustrated by Robert (2010). Davidson’s principles and practice of medicine(21st ed.). Edinburgh: Churchill Livingstone/Elsevier.
[15] Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Katus HA, Lindahl B, Morrow DA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasché P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S (October 2012). “Third universal definition of myocardial infarction”. Circulation. 126 (16): 2020–35.
[16] Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van ‘t Hof A, Widimsky P, Zahger D (October 2012). “ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation”. European Heart Journal. 33 (20): 2569–619.
[17] “AANS | Cerebrovascular Disease”. www.aans.org
[18] Degnan AJ, Gallagher G, Teng Z, Lu J, Liu Q, Gillard JH (September 2012). “MR angiography and imaging for the evaluation of middle cerebral artery atherosclerotic disease”. American Journal of Neuroradiology (Review). 33 (8): 1427–1435.
[19] Ropper, Allan H.; Adams, Raymond Delacy; Brown, Robert F.; Victor, Maurice (2005). Adams and Victor’s principles of neurology. New York: McGraw-Hill Medical Pub. Division. pp. 686–704.
[20] Caplan LR (September 1989). “Intracranial branch atheromatous disease: a neglected, understudied, and underused concept”. Neurology. 39 (9): 1246–50.
[21] Van Gijn, Jan; Kerr, Richard S; Rinkel, Gabriel JE (2007). “Subarachnoid haemorrhage”. The Lancet. 369 (9558): 306–318
[22] Juvela S, Porras M, Poussa K (May 2008). “Natural history of unruptured intracranial aneurysms: probability of and risk factors for aneurysm rupture”. Journal of Neurosurgery. 108 (5): 1052–60
[23] Maladies des vaisseaux, Éditions Doin, 1998, Joseph Emmerich,(ISBN 978-2-7040-0863-6)
[24] “What Causes Peripheral Arterial Disease?”. http://www.nhlbi.nih.gov/.
[25] “What Is Peripheral Arterial Disease?”. http://www.nhlbi.nih.gov/.
[26] López JA, Chen J (2009). “Pathophysiology of venous thrombosis”. Thromb Res. 123(suppl 4): S30–S34
[27] “What are the signs and symptoms of deep vein thrombosis?”. National Heart, Lung, and Blood Institute. 28 October 2011
[28] Ferri, F (2012). Ferri’s Clinical Advisor. St. Louis: Mosby’s
[29] Lewis, S; Dirksen, S; Heitkemper, M; Bucher, L (2014). Medical-surgical nursing: Assessment and management of clinical problems (9 ed.). St. Louis, MO: Elsevier Mosby. p. 552.
[30] Philip T. Cagle (2008). Color atlas and text of pulmonary pathology (2 ed.). Philadelphia: Lippincott Williams & Wilkins. p. 291.
[31] Goldhaber SZ (2005). “Pulmonary thromboembolism”. In Kasper DL, Braunwald E, Fauci AS, et al. Harrison’s Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 1561–65
[32] Kasper, Dennis L.; Fauci, Anthony S.,; Hauser, Stephen L.; Longo, Dan L.; Jameson, J. Larry; Loscalzo, Joseph (2015). Harrison’s principles of internal medicine. McGraw Hill Education. pp. 1593–1610.
[33] Dzau VJ, Atherosclerosis and hypertension: mechanisms and interrelationships, J Cardiovasc Pharmacol. 1990;15 Suppl 5:S59-64
[34] https://www.nhlbi.nih.gov/health-topics/atherosclerosis
[35] Sattelmair J, Pertman J, Ding EL, et al. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation 2011; 124: 789–795.
[36] Khosravi A, Akhavan Tabib A, Golshadi I, et al. The relationship between weight and CVD risk factors in a sample population from central Iran (based on IHHP). ARYA Atheroscler 2012; 8: 82–89.
[37] Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 2014: 63(25_PA).
[38] Unal B, Critchley JA and Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 2004; 109: 1101–1107.
[39] A. Virdis, C. Giannarelli, M. Fritsch Neves, S. Taddei and L. Ghiadoni. Current Pharmaceutical Design (2010) 16: 2518.
[40] Stewart J, Manmathan G, Wilkinson P. Primary prevention of cardiovascular disease: A review of contemporary guidance and literature. JRSM Cardiovascular Disease. 2017;6:2048004016687211. doi:10.1177/2048004016687211.
[41] NICE. Cardiovascular disease: risk assessment and reduction, including lipid modification. NICE Guideline CG181, 2016








![[Video] Eurosymposium on Healthy Ageing, Brussels, 2018 Eurosymposium on Healthy Aging](http://www.longlonglife.org/wp-content/uploads/2019/07/P1310252-218x150.jpg)